Detecting and Repairing Myelin Damage: ‘The Dawn of a New Era’

“Potential for myelin repair is there in the brain,” says Simons, winner of the National Multiple Sclerosis Society’s 2024 Barancik Prize for Innovation in MS Research for his work in myelin biology. “If you look in autopsy material of people with MS, around 20% of the lesions (damage areas or scars) do repair and 80% fail to do so.”For MS researchers around the world, two of their major research priorities are: detecting MS disease activity as early as possible, even before an MS diagnosis, and restoring myelin that has already been damaged.
Detecting Disease Activity Early
According to Christina Azevedo, MD, an associate professor of neurology at the University of Southern California, it’s important to detect MS at the earliest stage to prevent damage. Research suggests MS disease activity takes place years before someone has their first symptom.“If we can offer treatment as early as possible, then we'll be able to hopefully prevent long-term ramifications of the diagnosis,” Azevedo says.While researchers say detecting the disease as early as possible can be challenging, they are using several tools to help them, including biomarkers. Biomarkers are signals of disease process often found through blood or spinal fluid tests or imaging measures, like MRI. Azevedo says the recently revised McDonald Criteria (guidelines to diagnose MS) now incorporates 2 promising imaging biomarkers: the central vein sign (CVS) and paramagnetic rim lesions (PRLs) in lesions. She believes these biomarkers will help doctors diagnose demyelinating diseases like MS faster and more accurately.“Other diseases such as migraine or small vessel strokes should not cause the majority of lesions to have a central vein, whereas MS will,” Azevedo says. “If they're [PRLs] there in the right context, in a chronic state, we think that that could be more specific for demyelination.”Peter Calabresi, MD, director of the Johns Hopkins Multiple Sclerosis Center, helped revise the McDonald Criteria. He’s also conducted research on another promising MS biomarker known as neurofilament light chain (NfL). This protein is released in the blood and spinal fluid after nerves are damaged. Calabresi believes fluid biomarkers, like NfL, along with imaging biomarkers, can paint a clearer picture of disease activity for researchers.“The neurofilament adds that extra layer of specificity to tell us whether the tissue is actively being damaged,” Calabresi says. “Plus, we can use these tools to screen compounds that are going to be hopefully neuroprotective, or remyelinating in the future.”
The Potential for Myelin Repair and Regeneration
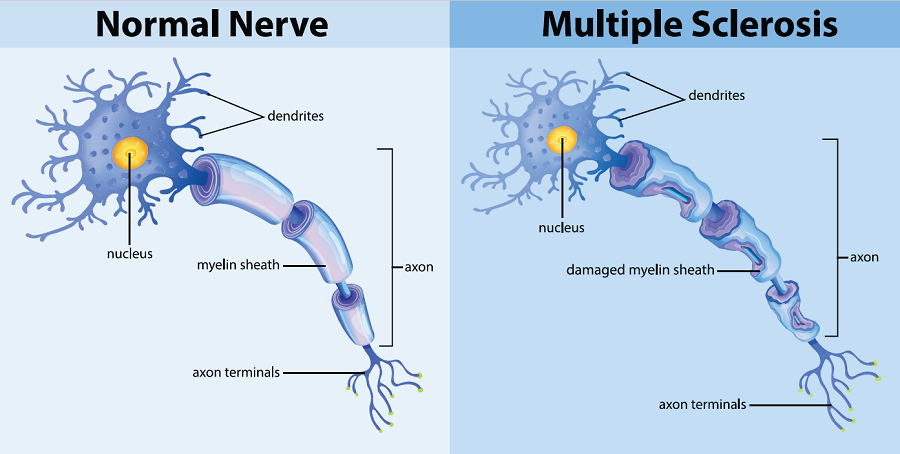
Whether it’s getting back on a bike or being able to focus while watching a movie, people with MS want to recover lost abilities. Researchers are taking a dual approach to restoring lost function. The first objective includes myelin sheath repair. This is called remyelination.Simons says to understand myelin sheath repair, “you have to understand how it functions normally.” He says after myelin is attacked, “reparative inflammation” occurs in the brain. This process is important for tissue repair and regeneration, and ends early in the disease process. Simons says this inflammation becomes chronic as MS progresses and prevents remyelination. He and his research team have identified several factors that cause this inflammation shift. For example, myelin debris forms after myelin is attacked. It must be cleared away before repair can begin. But Simons says the debris is rich in cholesterol and can’t be digested by brain cells (microglia). When the debris piles up, this leads to the bad inflammation synonymous with MS.