Relapsing-Remitting Multiple Sclerosis (RRMS)
Understanding Relapsing-Remitting Multiple Sclerosis (RRMS)
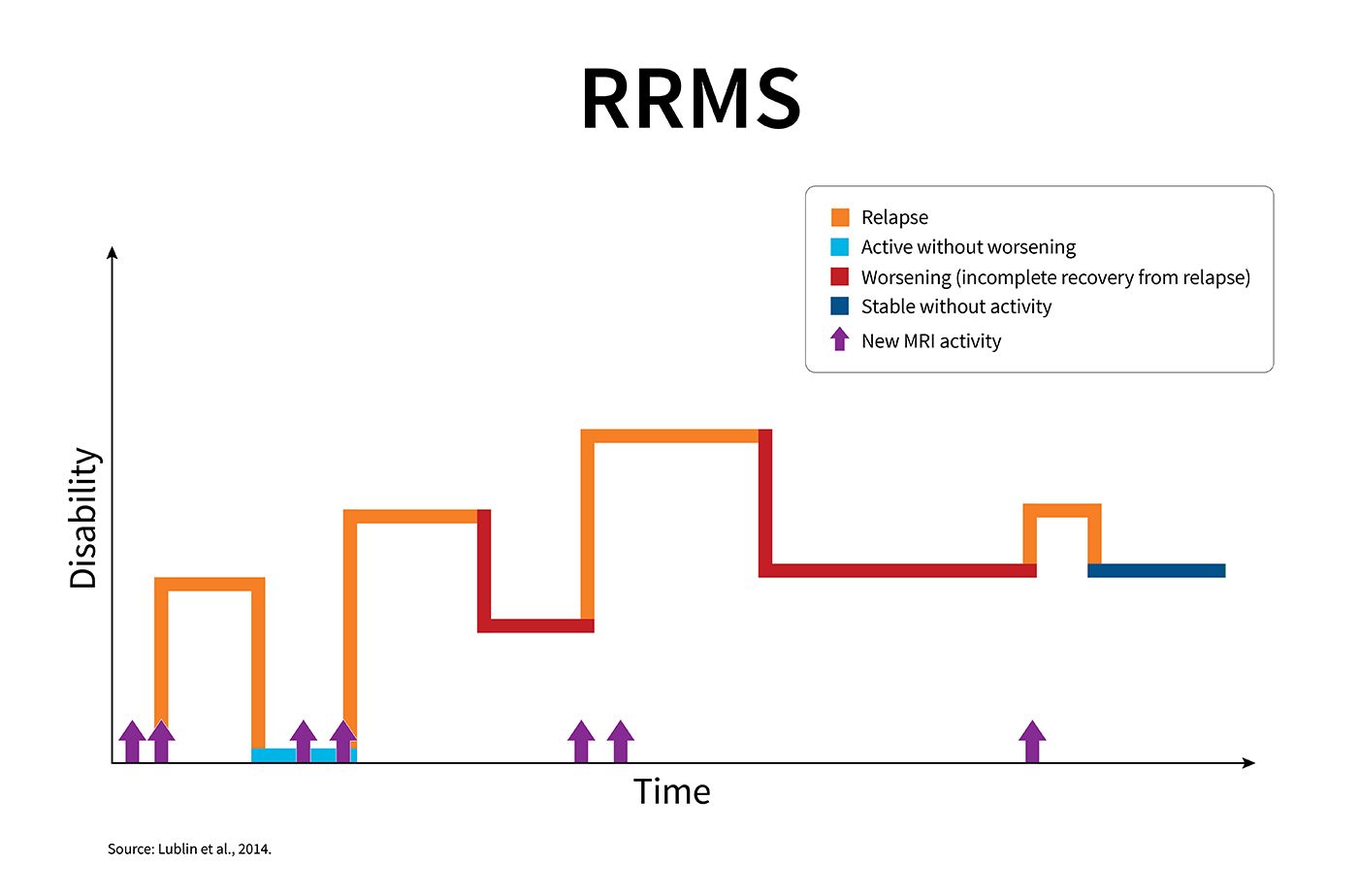
Multiple sclerosis is an unpredictable disease of the central nervous system that disrupts the flow of information within the brain and between the brain and body. Relapsing-remitting multiple sclerosis (RRMS) is the most common course of MS.If you have RRMS, you will experience clearly defined relapses of new or increasing neurologic symptoms. These relapses — also called "attacks” or “exacerbations" — are followed by periods of partial or complete recovery (remissions). During remissions, all symptoms may disappear, or some symptoms may continue and become permanent. However, there is no apparent progression of the disease during the periods of remission.RRMS can be characterized as either active (with relapses and/or evidence of new MRI activity over a specified period of time) or not active, as well as worsening (a confirmed increase in disability following a relapse) or not worsening.Approximately 85% of people with MS are initially diagnosed with RRMS.This graph shows the kinds of disease activity that can occur in RRMS, though each person's experience with RRMS will be unique. Following a relapse, new symptoms may disappear without causing any increase in level of disability, or new symptoms may only partially disappear, resulting in an increase in disability. New lesions on MRI, as shown by the arrows, often occur as part of a relapse. However, new MRI lesions indicating MS activity may also occur without symptoms of which the person is aware.
What Happens in RRMS?
RRMS is defined by inflammatory attacks on myelin — the fatty substance that surrounds and insulates nerve fibers (axons) — as well as the nerve fibers themselves. During these inflammatory attacks, activated immune cells cause small, localized areas of damage that produce the symptoms of MS. Because the location of the damage is so variable, no two people have exactly the same symptoms.Monitoring the Disease Course
Disease activity and worsening should be evaluated at regular intervals with a neurologic examination and magnetic resonance imaging (MRI). Being able to characterize the course of your disease at different points in time helps you and your MS care provider discuss your treatment options and expected outcomes.For example:- If you have RRMS that is active and worsening, you and your MS care provider may want to discuss a different treatment approach than if there were no evidence of activity or worsening. Together, you can weigh the potential risks and benefits of other treatment options.
- If your symptoms have not worsened while on your current treatment, but you have evidence of new disease activity on your MRI, you and your healthcare provider may discuss switching to another treatment with a different mechanism of action to control the disease activity more effectively and help prevent worsening.
- If your RRMS is stable without evidence of MRI activity or worsening, you and your healthcare provider can feel confident that the current treatment regimen is working effectively.
How RRMS Differs From Progressive Types of MS
While RRMS is defined by attacks or relapses of new MS symptoms, progressive forms of MS involve fewer attacks and are characterized by gradual accumulation of disability. In addition:- People with RRMS tend to develop more new brain lesions — also called “plaques” or “scars” — on magnetic resonance imaging (MRI) scans. People with primary progressive MS (PPMS) tend to have more spinal cord lesions.
- People with RRMS tend to have more inflammatory lesions on MRI (seen when gadolinium dye is used during the MRI).
- In RRMS, women are affected two to three times as often as men. In PPMS, the number of women and men diagnosed is approximately equal.
- Most people with RRMS are diagnosed in their 20s and 30s (although it can occur in childhood or later adulthood) while PPMS is typically diagnosed during the 40s or 50s.
- The transition from RRMS to SPMS generally occurs in people who have been living with RRMS for at least 10 years.
RRMS Symptoms
The most common symptoms reported in RRMS include bouts of:- Bowel and bladder problems
- Fatigue
- Numbness
- Problems with cognition (learning and memory or information processing)
- Spasticity or stiffness
- Vision problems
Diagnosing RRMS
The criteria for diagnosing relapsing-remitting MS require evidence of at least two separate areas of damage (“dissemination in space”) in the central nervous system that have occurred at different points in time (“dissemination in time”). The diagnostic criteria utilize MRI results in combination with a history of symptoms as well as findings on the neurological examination to help make the diagnosis. In addition, the doctor must be able to rule out any other diseases or conditions that might be responsible for the symptoms.Recent changes to these criteria allow the presence of a specific group of proteins cerebrospinal fluid to substitute for "dissemination in time," thereby speeding up the diagnostic process for many people.
Treating RRMS — Modifying the Disease Course
The Food and Drug Administration (FDA) has approved more than 20 medications— also known as disease-modifying therapies or DMTs—to treat relapsing forms of MS. These relapsing forms are clinically isolated syndrome (CIS), relapsing-remitting disease (RRMS) and active secondary progressive disease (SPMS with relapses).Research has shown that all the MS medications can:- Reduce the number of relapses (also called attacks or exacerbations)
- Limit new MS activity (new areas of damage called plaques or scars) in the central nervous system as seen on magnetic resonance imaging (MRI)
- Slow disease worsening (progression)