Secondary Progressive Multiple Sclerosis (SPMS)
Understanding Secondary Progressive Multiple Sclerosis
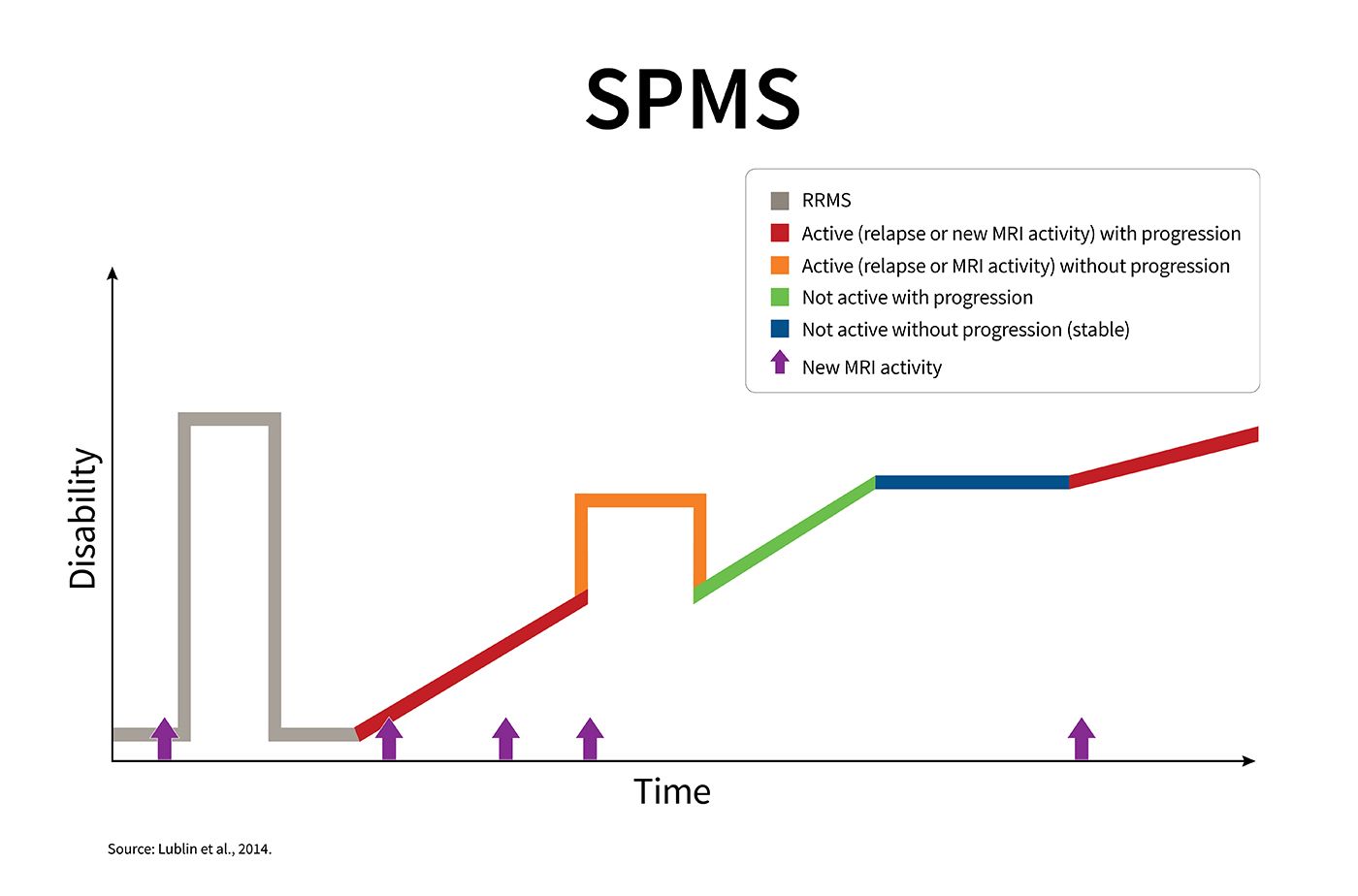
Multiple sclerosis is an unpredictable disease of the central nervous system that disrupts the flow of information to and from the brain. There are 4 disease courses in MS. Secondary progressive multiple sclerosis (SPMS) follows the initial course of relapsing-remitting multiple sclerosis (RRMS). Some people who are diagnosed with RRMS eventually go on to have a secondary progressive course, in which neurologic function worsens over time and disability increases. According to estimates, in the United States, the prevalence of SPMS is 27–45 for every 100,000 members of the general population.SPMS can also be described as active (with relapses and/or evidence of new MRI activity during a specified period of time) or not active, as well as with progression (evidence of more disability over time, with or without relapses or new MRI activity) or without progression.This graph shows the kinds of disease activity that can occur in SPMS, though each person’s experience with SPMS is unique. As the graph shows, following a period of relapsing-remitting disease, your disability may increase over time, with or without evidence of disease activity (relapses or changes on MRI). You may also have occasional relapses, as well as periods of stability.
Common Signs and Symptoms of Secondary Progressive MS
If you have SPMS, you will experience a gradual, steady change in your ability to do things over time. But one person’s symptoms may progress differently or at a different rate than someone else’s.Symptoms of SPMS include:
- Bowel and bladder issues, such as an urgent need to urinate
- Difficulty with walking and coordination
- Fatigue
- Numbness or tingling
- Problems with cognition, such as learning, remembering information or processing it
- Spasticity or stiffness of the muscles
- Vision problems
Monitoring the Disease Course
Your disease activity and progression should be evaluated at least once a year by your MS healthcare provider. The evaluation should include a discussion of your symptoms, a neurologic exam and possibly an MRI. Characterizing the course of your disease at different points in time helps you and your MS care provider discuss your treatment options and expected outcomes.For example:
- If you have SPMS that is active, you and your MS care provider might talk about starting treatment with a disease-modifying therapy (DMT) to reduce the risk of a relapse.
- If you have SPMS that is active and progressing despite the medication you are taking, your conversation with your MS care provider might be about the potential benefits and risks of switching to a more aggressive treatment strategy.
- If you have SPMS that is not active but is progressing with increasing disability, you and your MS care provider might focus on rehabilitation strategies to help improve your function and mobility, as well as to promote safety and independence.
- If you have SPMS that is stable and is not active or progressing, you and your MS care provider might focus on rehabilitation and other symptom management strategies to help you maintain function.